Frontline Medicine
Ali Amini helped out in early February with clinical shifts out of hours whilst still a full-time DPhil student. This included going to people’s homes in full PPE with a paramedic as part of the home-swabbing programme rolled out in the containment phase of the pandemic.
After lockdown, he paused his DPhil and went back to the NHS full-time for a few months, working on the John Radcliffe COVID-19 and Infectious Diseases wards, as well as contributing to some of the research in the hospital.
In June 2020 Ali returned to his DPhil, helping process COVID-19 bloods regularly as part of the ‘Oxford Immunology Network COVID-19 response: T cell Immunity Team’ at the Peter Medawar Building. He also helped with research projects looking at the immune response of vaccinated patients.
His DPhil pre-pandemic was on the immune response to respiratory viruses and vaccine vectors (ChAdOx1); ChAdOx1 is particularly topical as it is the backbone of the Oxford COVID-19 vaccine.
During lockdown Isobel Argles helped her supervisor (Tammie Bishop) with a project looking at whether the HIF pathway is involved in the regulating the expression of the SARS-CoV-2 receptor ACE2. This is with a view that if it is involved, clinical agents that modulate the HIF pathway might be useful as either prophylactic measures or treatments for COVID-19.
Jessica Caterson worked in the Royal Berkshire Hospital in Reading in the Intensive Care Unit. Whilst she was there she helped with three projects.
Jessica was particularly involved as an incoming junior doctor in the GenOMICC Study and was the major contributor to the screening of, consenting of, and collecting blood samples from, patients who were either on ICU, or had been stepped down to wards from ICU. The purpose of the study was to determine if there was any genetic preponderance to becoming critically unwell with SARS-CoV-2. She was responsible for 90% of recruitment at the Royal Berkshire Hospital (RBH). RBH was, at its peak, an overall top five recruiter (second place for patients per bed spaces), and remained in the top ten over late April/May during the peak of the pandemic.
She was also involved in the Recovery Trial which was responsible for the breakthrough regarding dexamethasone in treating COVID-19.
In addition, Jessica worked on PRIEST, an Urgent Public Health Study, prioritised by the Department of Health and Social Care as part of the Government’s research response to COVID-19pandemic. The aim of the PRIEST study was to optimise the triage of people using the emergency care system (999 ambulance or hospital emergency department) with suspected respiratory infections, namely coronavirus, and identify the most accurate triage method for predicting severe illness among patients attending the emergency department with suspected coronavirus.
Andreas Halner’s DPhil research is interdisciplinary, applying machine learning in order to develop a variety of predictive tools for chronic obstructive pulmonary disease. He is also co-founder and chief operating officer of the start-up Oxford Cancer Analytics which seeks to detect cancer early through machine learning-based analysis of blood samples.
At the end of March Andreas and his supervisor engaged in one week of research into global patterns of inhaled corticosteroid (ICS) use. Understanding ICS use patterns might be significant because of the interesting observation in a number of studies that severe cases of COVID-19 are less prevalent than expected in patients with chronic lung diseases, leading to the hypothesis that ICS, which are routinely used by patients with chronic lung disease, may help reduce COVID-19severity. If the Oxford-based STOIC trial confirms this, then ICS could be prescribed to patients in the early phase of COVID-19 illness to help avoid severe symptoms. Andreas familiarised himself with the STOIC trial protocol and began helping doctors and nurses with the STOIC trial by helping record details from phone-based STOIC patient conversations.
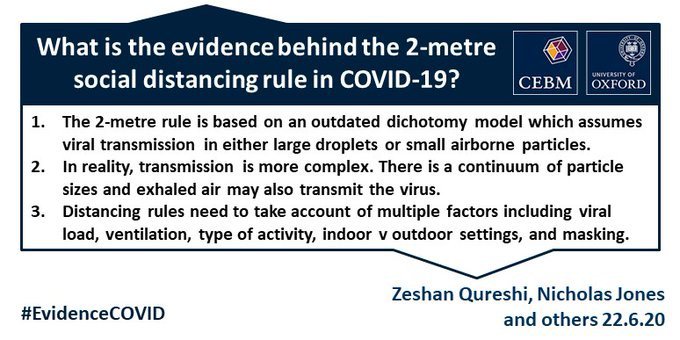
Jessica Larwood worked with the Centre for Evidence Based Medicine and Lydia Bourouiba from MIT and published a critical review of the 2-metre rule.
Jessica also worked on the COVID-19 Vaccine Trial from the beginning of lockdown. She helped on the ground in Oxford and then switched to working as the Project Manager for Sheffield, helping them to set up their vaccine trial site. She also contributed to writing the 'Standard Operating Procedure for Vaccine Management', creating training packages for the sites, sourcing supplies and organising the distribution of them, and creating and reviewing trial documents.
Omar Abdel Mannan published a paper on neurological manifestations in children with COVID-19 at Great Ormond Street Hospital.
He has also been appointed to a one-year research Fellowship at UCL institute of neurology on paediatric multiple sclerosis.
Liam Peck started lockdown by volunteering as a driver for an impromptu food bank and pharmacy delivery service (Dons Local Action) near his home in Wimbledon, set up by the AFC Wimbledon Football Club. He found it to be a really impressive operation across a large area of south-west London.
On his return to Oxford he was heavily involved in the day-to-day management of the Oxford University Hospitals staff COVID-19 screening programme, which routinely screens the 10,000+ staff members across four hospital sites. As part of this work, he was also seconded to work at the Europa school in Oxfordshire on the ‘COVID-19surveillance in Kids’ (sKID) pilot trial for similar viral screening in schools. The trial was commissioned by Public Health England to inform the government’s decisions about a safe return to schools and ongoing virus screening in schools from September onwards.
Liam also featured in a song for Christmas from the NHS, put together by medical student society Tingewick as part of the Oxford Hospitals' Christmas message to staff.
Ankit Ranjan worked with Curative in Los Angeles, which ran approx. 7% of the tests in the USA. He was also involved in starting their vaccine trial.
In addition to working on the Oxford University Hospitals staff-testing scheme, Thomas Ritter worked as part of the ISARIC4C team, one of the UK-wide NIHR Urgent Public Health Priority studies for hospitalised patients with COVID-19. His role was to assist the research team in collecting samples from patients from a wide array of hospital settings, including from ICU, and then transporting these samples to the multitude of labs that are running the investigations
He commented:
‘I have been fortunate enough to meet and interact not only with patients but also front-line research staff from the OUH trust, colleagues at CCVTM, the Peter Medawar Building for Pathogen Research, and the Wellcome Centre for Human Genetics. Truly integrating into this multidisciplinary team, and being able to contribute in a meaningful way to work that is producing an extensive amount of results that will shape future treatments and policies, has been immensely rewarding, and hopefully these friendships and collaborations will continue long after we emerge from the current global pandemic.’
Thomas also travelled to Bradford to play a part in unravelling a mystery: the curious case of a choir, who in January had many members suffer from a mysterious pneumonia-like disease, as documented by Professor John Wright for the BBC. Thomas connected a handful of these choir members with the research teams he had been working with and took samples from them. The work was to investigate if potentially the unknown disease was in fact SARS-CoV-2, making the choir the first case of COVID-19 in the UK.
- Worked on a clinical research audit with Dr Robert Shaw in the microbiology department, logging the timeline of symptoms of all the patients with suspected or confirmed COVID-19. This database was used to inform trust pathways for CXR testing.
- Contributed to a paper reviewing the guidelines for remote consulting in the post-COVID-19 era supervised by Mr Peter Kalu (plastic surgeon at the John Radcliffe Hospital).